Because one-of-a-kind doesn’t fit all
SDOH solutions support purpose-driven health. Addressing social determinants can increase access to healthcare and improve quality measures across organizations.
Research confirms economic, social, environmental, educational, and health differences affect people in various ways. Similarly, differences exist in health and social care providers’ needs, goals, and priorities. Bringing people and organizations together can create a beautiful vision for the future, like making a NinePatch quilt.
At NinePatch, we realize that one-size-doesn’t-fit-all when evaluating social determinants of health interoperability solutions. A focus on client needs is a priority of our software development efforts to create SDOH solutions that support collaboration and verifiable results for clinical and social care organizations.
NinePatch® SDOH Solutions
Patient and social care improves by collaborating, sharing, and exchanging electronic health information. NinePatch® Whole Person Care, RIE™, and NinePatch® Community Convener Services are complementary SDOH solutions.
Organizations can use the software solutions for care coordination, consents, and closed-loop referrals. Convener services provides on the ground support in local communities for program implementation, partnership building, governance, and financial sustainability.
There are many ways that NinePatch software supports interoperability between healthcare and community-based organizations, here are a few:
-
- The second-generation digital health platform links healthcare organizations, payers, patients, and community organizations to simplify care coordination
-
- White-labeled and customizable SDOH software gives organizations the power to share data to analyze and report social and clinical outcomes
-
- Bi-directional data sharing, intake, assessment, robust consent management, and other software features enhance workflow efficiencies
NinePatch® Simplifies Coordinating Health and Social Care
Social determinants of health impact daily life beginning in childhood and extending to adulthood and advanced age. NinePatch Whole Person Care—featuring the OneView, a Robert Wood Johnson award-winning design—combines health, social, and behavioral components to address SDOH-related concerns.
Identifying and matching needs across healthcare ecosystems by using SDOH solutions delivers better results when patients and clients are active participants.
-
- Assessment tools identify what’s essential or time-sensitive so that care plan coordination provides access to the right providers and support at the right time.
- Data-sharing between in and out-of-network providers reduces repetition and duplication of effort especially when patients’ journeys take them from a doctor’s office to an imaging center to a housing support agency.
- The document vault stores patient records, personal documents, and care plan information to reduce the time required to qualify clients for services.
- The robust consent model provides access at the right level for the right users.
Consents When and Where Needed
For example, a community health manager at a food bank may have access to social but not medical or behavioral health information. On the other hand, a doctor at a community health center has access to the entire OneView identifying health, medical, and social needs.
Additionally,
-
- Rapid referrals are sent and received in minutes instead of hours, increasing the providers’ available time to help more people—no more spending hours on the phone, faxing, or waiting to confirm service availability.
- ADT (admit-transfer-discharge) notifications mean that providers can follow up promptly knowing when patients are admitted or discharged from the hospital.
Having the right SDOH solutions at your fingertips means that coordinating health and social care doesn’t require more programs, time, or extra effort. NinePatch product design creates user-friendly software applications.
How Social Determinants Relate to Health and Well-Being
Community healthcare workers meet with clients daily who struggle to fulfill basic needs like access to nutritious foods, transportation, or steady employment. Unfortunately, the stress associated with meeting daily needs or accessing public health services results in emotional stress and increases the likelihood of chronic illness.
With so much to juggle, trade-offs between paying the electric bill, buying groceries, picking up a prescription, or attending doctor appointments can result in hard choices for individuals and families. As a result, risk factors and costs related to poor health can skyrocket.
Patients who are economically disadvantaged, uninsured, or without a regular physician are 40 to 80% more likely to delay receiving care eventually leading to hospitalizations with longer stays and potentially poorer health outcomes. (1)
Underserved Populations May Not Seek Medical Care
The staff at community-based organizations are more likely to work with underserved and vulnerable persons who may not seek medical care but need food, transportation, housing, or other support. Gaining access to healthcare can be a struggle when working to pay the rent or buy food is more of a necessity.
Together, hospitals, health systems, healthcare, and community organizations can build partnerships to use SDOH solutions to address income, food, transportation, and other social concerns affecting chronic disease management and hospitalizations.
With whole person care and referral information exchange software, providers have information about the organizations and individuals involved in patient and client care at their fingertips.
When SDOH assessments become routine, having a network of care means that needed services are delivered. Patient and client follow-ups become routine instead of emergency-based, thereby lowering costs and improving care.
90% of the nation’s $4.1 trillion in annual health care expenditures are for people with chronic disease and mental health conditions
The Link Between Chronic Disease and SDOH
According to the CDC, chronic diseases have high economic and health costs.
-
- The ICD-10 code for food insecurity, 259.41, relates to SDOH factors associated with inadequate food. Poor nutrition or lack of access to food poses negative implications for persons struggling to manage diabetes or heart disease.
- Experiencing a natural disaster—like a hurricane, earthquake, or tornado—
can result in physical injuries and result in Z59.0 homelessness or Z59.1 inadequate housing. Both of these social factors can worsen physical or mental health conditions.
When the unexpected happens, emergency health providers and community organizations, like food banks and homeless shelters, coordinate with healthcare systems and providers. Especially in time sensitive situations, provider access to SDOH solutions simplifies care coordination for families and individuals experiencing a wide variety of needs.
Transportation is a Barrier to Receiving Medical Care
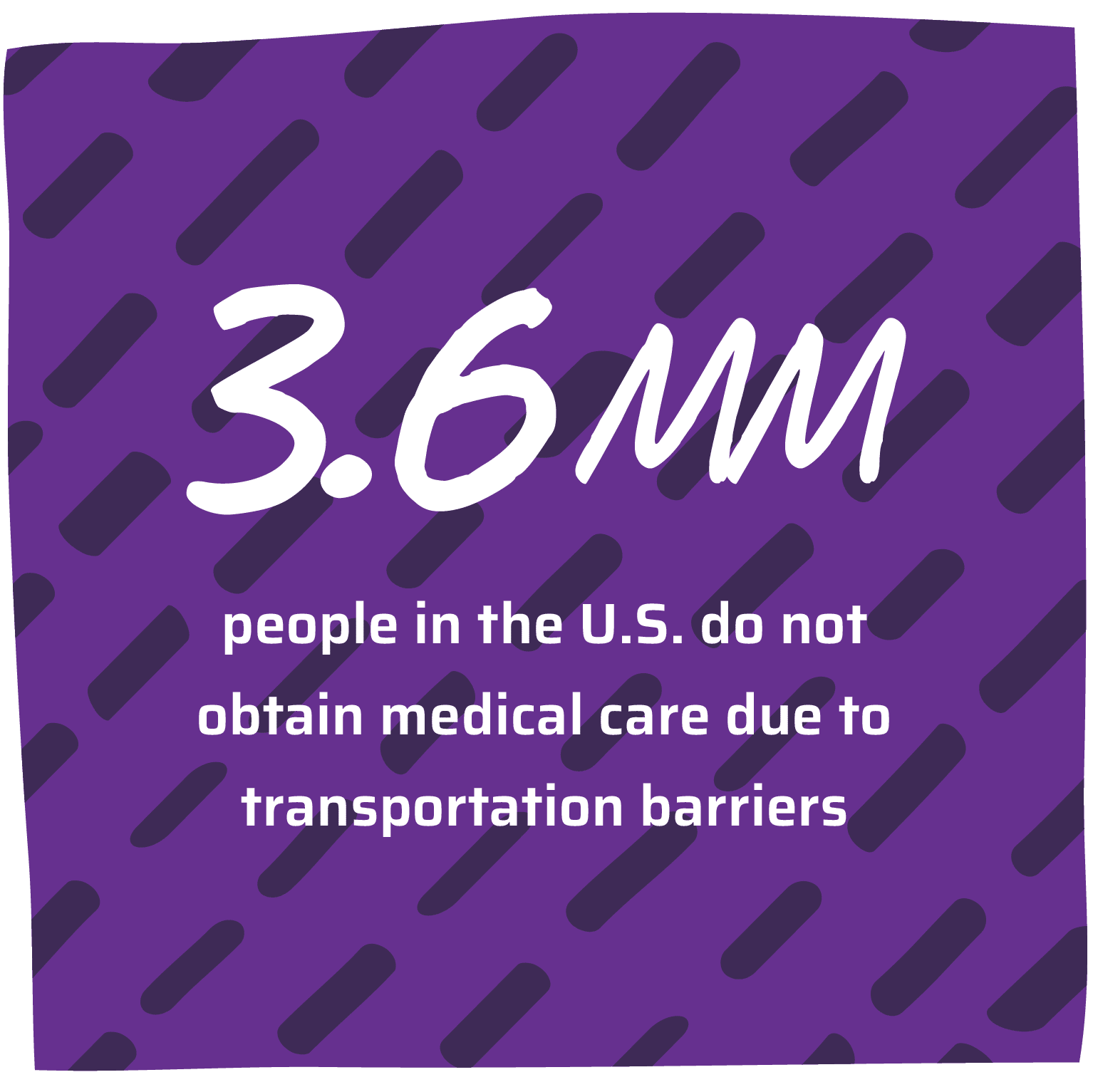
Transportation is the third most commonly cited barrier to accessing health services for older adults. 3.6 million people in the U.S. do not obtain medical care due to transportation challenges.
-
- SDOH data confirms that a lack of transportation adversely impacts access to health services and makes it difficult to manage health conditions.
- Missed doctor and clinic appointments, physical disabilities, and the inability to fill prescriptions increase financial costs for healthcare systems that treat patients sicker and quicker.
Transportation affects individual’s ability to work, obtain medical care, and access essential needs like groceries. When local communities improve access to close transportation gaps, this means that vulnerable patients, the elderly, and everyone can participate in health and community services to enhance daily life.
Community Collaboration and Interoperable Solutions Reduce Health Disparities
NinePatch SDOH solutions facilitate interoperability between health and social systems using clinical and social determinants of health data to substantiate outcomes and meet quality measures that support funding and reimbursements.
Providing value-based care will remain a priority for healthcare systems. Combining efforts with community-based organizations makes providing high-quality care more cost-effective. Join with NinePatch to reduce health disparities, improve health, and create healthier communities.
